Shoulder calcification is a common pathological condition of the shoulder joint, which mainly affects the population in the 30–50 age group, and occurs more often in women. Risk factors for the development of shoulder calcification include diabetes, previous shoulder injury, especially to the muscles and tendons of the rotator cuff, or shoulder dislocation, incorrect posture, and prolonged immobilisation of the arm, e.g. after a fracture.
There are two types of shoulder calcification: degenerative calcification of the shoulder in reactive calcification of the shoulder. The first is typical for the elderly and occurs gradually due to the loss of quality of collagen fibres in the connective tissue of the shoulder and the gradual formation of microinjuries. Reactive calcification of the shoulder occurs as a result of previous injury, trauma, thyroid problems, or in conjunction with other typical risk factors.
If not treated with appropriate physiotherapy, shoulder calcification can develop into frozen shoulder syndrome, which causes more severe shoulder pain.
The condition of shoulder calcification is characterised by a three-phase cycle that can last up to five years, and if hormonal disorders are present and no treatment is performed, it can last up to eight years.
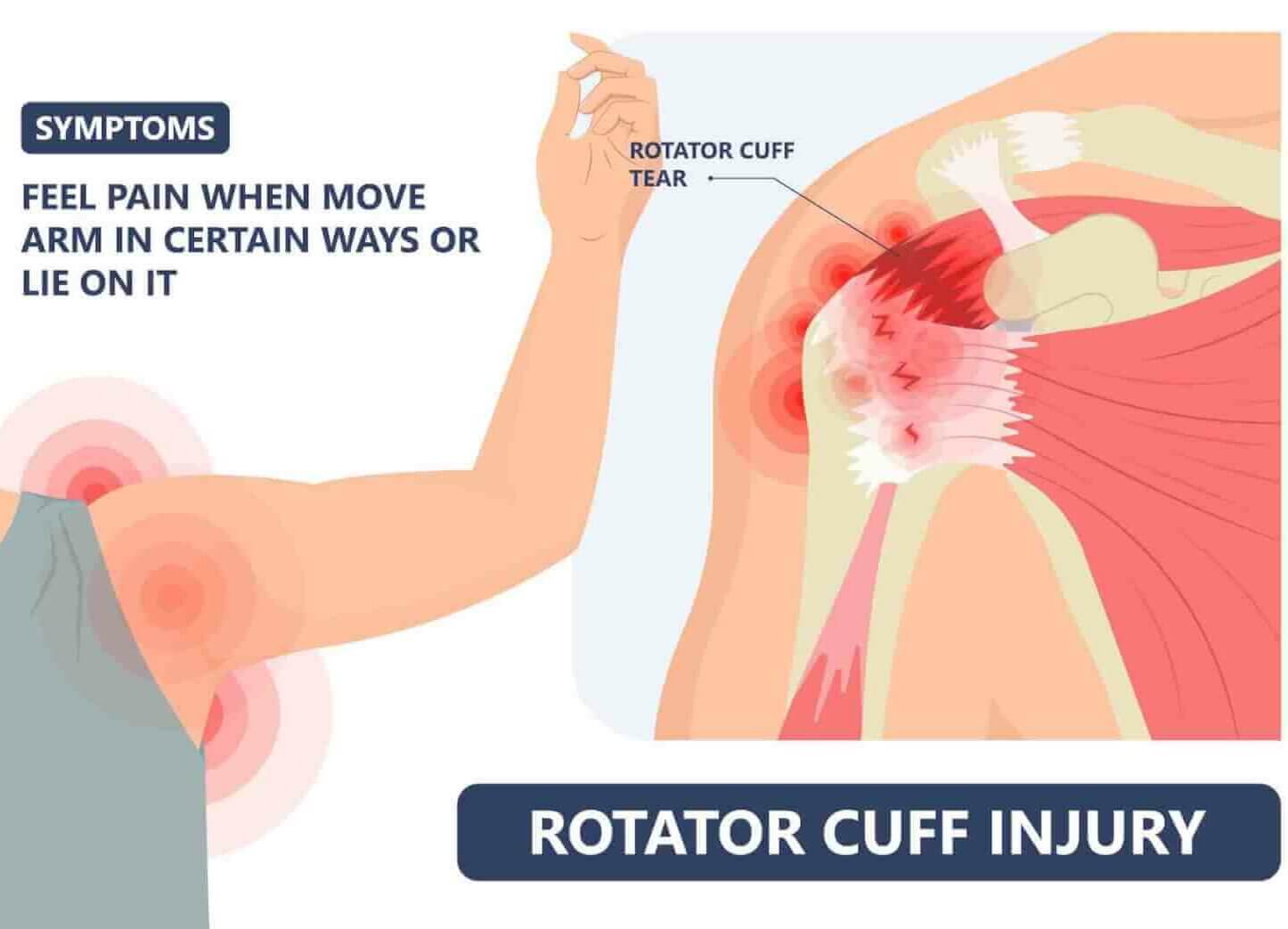
Shoulder calcification is characterised by pain that worsens with rest and immobility of the shoulder. Night-time pain is typical, disrupting sleep and causing intense pain when lying on the affected shoulder. Pain from shoulder calcification usually begins suddenly, is sharp, and limits movement of the arm above the head. Often, a standing position is more pleasant for patients with shoulder calcification than a lying position.
Shoulder calcification is characterised by intense pain in the front or back of the shoulder, which often radiates into the upper arm, possibly to the elbow and wrist. If you also have tingling in your fingers, it is not a problem related to shoulder calcification, but there is suspected carpal tunnel syndrome.
Shoulder calcification develops in three phases; the third phase is the most painful, when calcium crystals are released from the tendon into its surroundings. Physiotherapy and kinesiology are usually performed in the third phase of shoulder calcification, as it is asymptomatic in most cases before this stage, which means that we do not have contact with patients at that time.
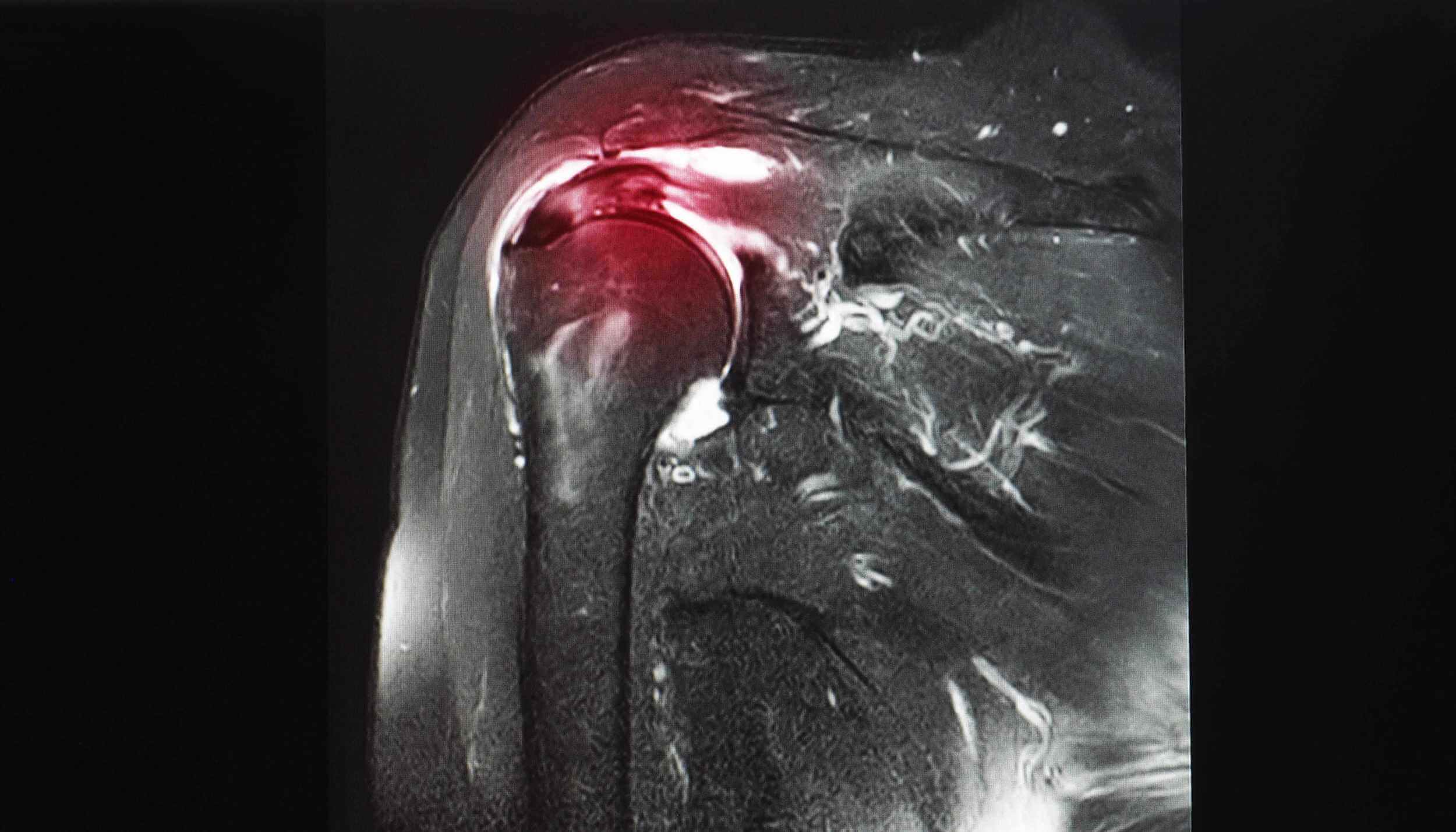
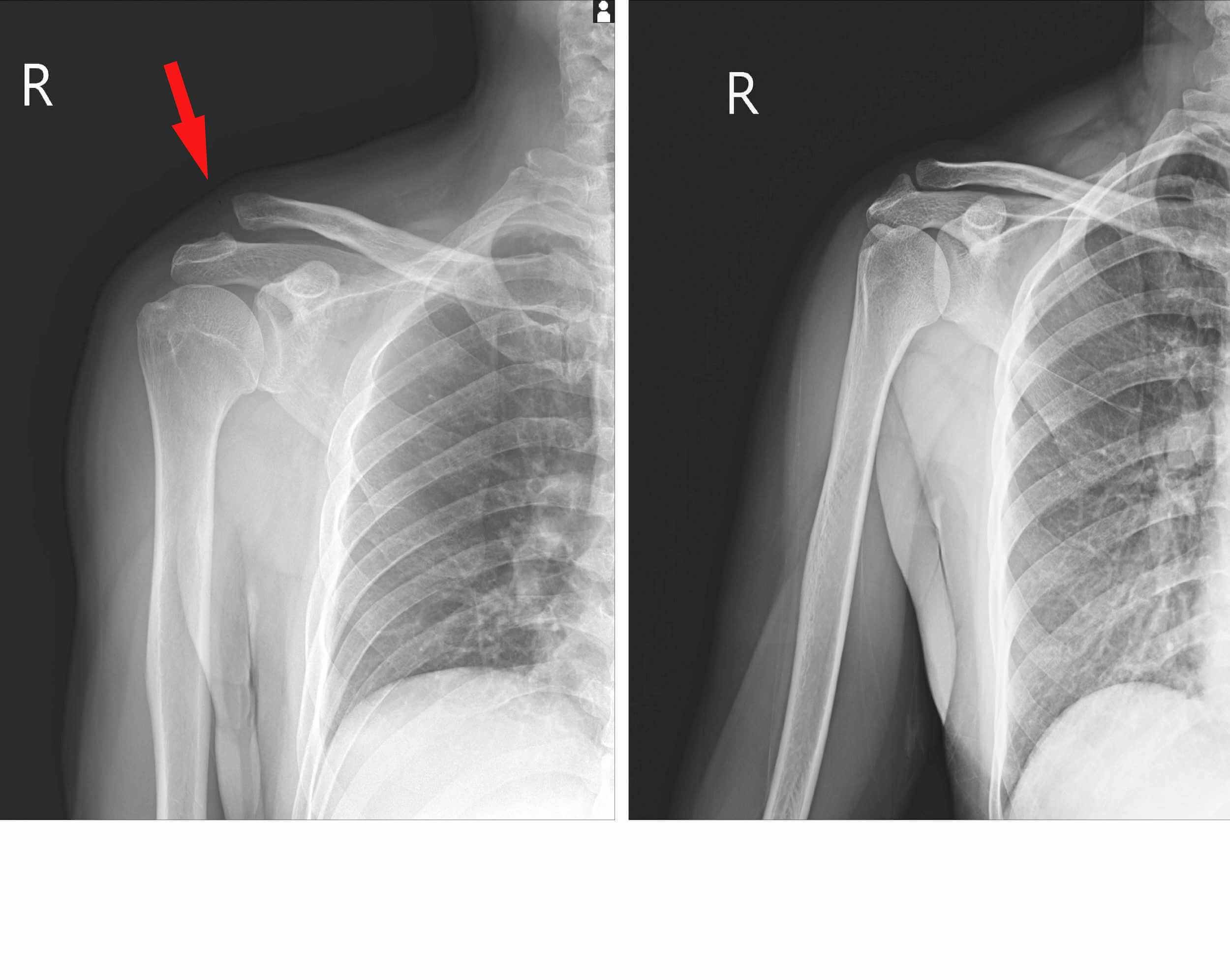
A reliable diagnostic method for examining the shoulder where calcifications are suspected is an ultrasound examination (US) by a radiology specialist. Ultrasound imaging precisely determines the location of calcium crystals and their size, and can also be used as a method of monitoring the progress of conservative treatment of shoulder calcification.
Treatment of calcifications in the shoulder is complex, and requires a comprehensive conservative approach combining physiotherapy and kinesiology. Surgical treatment is only performed in 5–10% of patients when physiotherapy treatment is unsuccessful after at least nine months of continuous rehabilitation.
The primary physiotherapy method for treating shoulder calcification is extracorporeal shockwave therapy combined with active shoulder mobilisation and rotator cuff strengthening exercises. TECAR and LASER therapy are also used, as well as electrotherapy, which must be high-tone – at Medicofit clinic, we use HiToP. Treatment of shoulder calcifications should also include exercises to develop overhead pushing and pulling strength in the final phase, as failure to gain strength in the final ranges of overhead movements poses a risk of recurrence of calcifications.
It is important that the treatment is combined in every therapy, extracorporeal shockwaves must be precisely measured in intensity and must not trigger an intense pain response to the therapy, despite the fact that they are among the more invasive methods of instrumental therapy. Extracorporeal shockwaves are the most effective means of conservative treatment of shoulder calcification, but they must always be accompanied by special exercises that strengthen key muscle groups.